Quick Summary
Healthcare businesses have evolved to add sophisticated processes, new-age technologies, and advanced analytics to make their businesses more competent and agile. This is where healthcare dashboards that provide visual analytics and insights of business metrics, patient outcomes, and financials are now top priorities of healthcare organizations. These dashboards display critical KPIs that are required for healthcare business decision-making.
Providers, Payers, Medtech, and Life Sciences are overwhelmed with data derived from electronic health records (EHRs), claims processing systems, medical devices, clinical trials, and regulatory reports. However, this data is scattered and not centralized. This can reduce the efficiency with which healthcare organizations analyze data for insights. Also, more time spent in these data analysis workflows can affect & divert attention from the most critical aspect— patient care analytics.
This is why healthcare organizations need to know the most critical KPIs that they need to prioritize. Also, implementing sophisticated business intelligence tools like Power BI healthcare dashboards that can be customized to measure KPIs as per the specific needs of diverse healthcare organizations.
“In this blog, we bring the 10 healthcare data dashboard examples and must-know healthcare KPIs for powerful and insightful dashboards.”
10 Must-Track KPIs for Comprehensive Healthcare Dashboards
Gartner highlights identifying redundancies, improving information relevance, building cross-functional collaboration, and investing in skills development as the ways to tackle challenges related to scattered data scenarios. Top healthcare business intelligence tools like Power BI healthcare dashboards display essential KPIs & metrics critical in transforming raw data into actionable insights, allowing real-time decision-making, improving healthcare workflows, and ultimately improving patient outcomes.
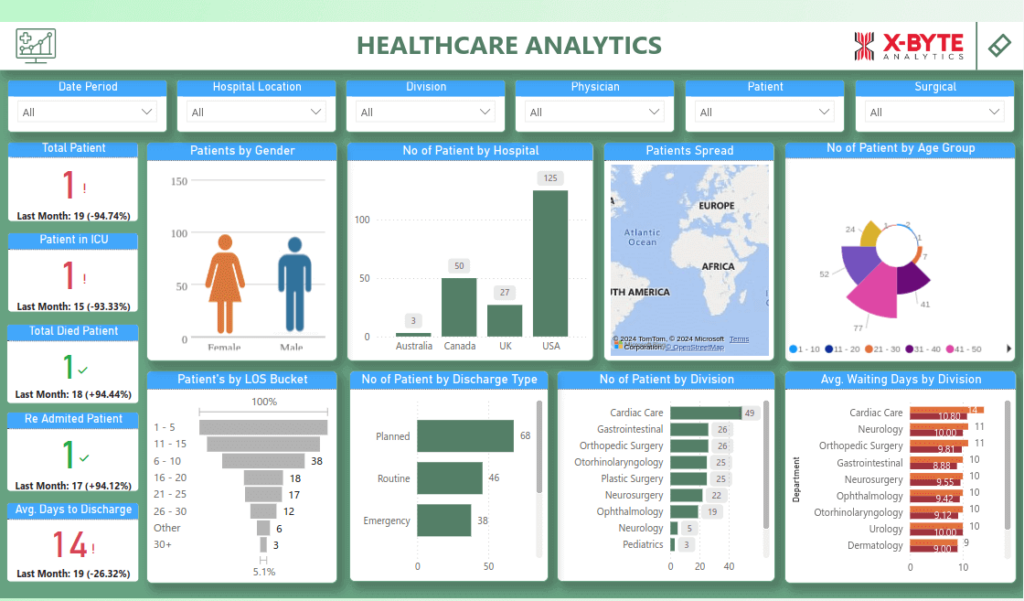
Image Source: Healthcare Dashboard
Let us study the 10 key metrics and KPIs important for healthcare business monitoring & intelligence.

1. Patient Satisfaction Score
Patient satisfaction is a complex task for providers and payers, and achieving it is amongst the top agendas of healthcare organizations, which can be achieved with a healthcare provider dashboard with a patient satisfaction score. This is substantiated by McKinsey’s survey where it was found that satisfied patients are 28% less likely to switch providers. Consumer-centric healthcare companies have the chance to double their revenue as compared to competitors with lower patient satisfaction scores.
- What it Measures: While healthcare organizations may put in their best efforts, it needs to be validated by the patients themselves. A dashboard displaying the patient satisfaction score can help providers gain a perception of care quality and service experience.
- Why it Matters: Patient satisfaction scores are particularly important as they show the probability of a patient being retained. It also acts as a mirror to the perception of the hospital by the patients and can affect the hospital’s reputation.
- How to Calculate: Healthcare patient satisfaction dashboards can be built around patient surveys, post-visit feedback, or patient reviews like the HCAHPS scores.
- Impact on Healthcare Outcomes: Access to the patient perception can help providers and payers improve patient care, and reduce any legal risks that may come up.
- Best Practices: The incorporation of patient satisfaction scores through dashboards is enabled by real-time feedback systems that help address recurring issues and deliver better patient care.
2. Average Patient Wait Time
For patients going through agony and suffering, long wait times can be annoying. A McKinsey survey states that two-thirds of those surveyed sought care with some other provider when they faced a long wait time with their current provider. Providers must address this concern by getting insights into the average wait time and taking steps to ensure a faster healthcare onboarding process.
- What it Measures: The average patient wait time signifies how much time a patient has to wait before they get access to their healthcare professional and healthcare.
- Why it Matters: A longer average patient wait time can either be an indicator of an overwhelmed healthcare ecosystem, improper planning, or a need for a tweak in appointment scheduling. All these not only impact patient satisfaction, but also are an indicator of inefficiency in operations.
- How to Calculate: The average wait time is calculated by dividing the total wait time by the number of patients. The higher the result displayed on the Power BI healthcare dashboard, the more important it becomes for healthcare organizations to make plans accordingly for better patient satisfaction and results.
- Impact on Healthcare Outcomes: A shorter wait time is often an indicator of an efficient system where patient care is prioritized and can lead to better patient retention and care efficiency.
- Best Practices: When the average wait time is monitored through dashboards, healthcare professionals can make adjustments to appointment scheduling, and improve staff efficiency, while reducing bottlenecks.
3. Net Revenue
Healthcare organizations work on a global scale and are loaded with complexities related to contractual rates, and billing inaccuracies, which can altogether lead to inaccurate revenue projections. Hence, it becomes imperative to have real-time data and forecasts, and a Power BI healthcare dashboard displaying net revenue KPI can be a lifesaver, as it helps gauge the financial viability of their organization’s revenue cycle.
- What it Measures: A healthcare ROI dashboard with net revenue KPI adds insight into the revenue expenses, including patient care, billing, and insurance.
- Why it Matters: The sound financial health of a healthcare organization is a step towards ensuring the health of the patients. A healthcare executive dashboard metrics that reflect the revenue earned helps the organization to include technological innovation and other resources while ensuring ROI.
- How to Calculate: Broadly, the expenses incurred operating the organization and other miscellaneous expenses are subtracted from the overall revenue to arrive at a figure.
- Impact on Healthcare Outcomes: When the revenue is in the positive zone, the healthcare organization can deliver better access to medical facilities and can incorporate better medical equipment, thus ensuring the overall benefit for the organization, staff, and patient care services.
- Best Practices: The healthcare KPI dashboard with the revenue details can help in performing regular financial audits and effective billing strategies.
Get tailored healthcare dashboards that track KPIs from patient satisfaction to financial metrics!
4. Cost Per Treatment
A healthcare organization can perform better when it knows how much a treatment is going to cost for a particular patient. Using cost-per-treatment KPI dashboards, medical billing dashboards, and clinical performance dashboards, providers and payers can identify avenues for saving and investments. A Power BI healthcare analytics dashboard integrated with third-party data can give an in-depth analysis of real-time insights on medical products, geographic segments, etc., and can help develop investment strategies accordingly.
- What it Measures: The dashboard with a view into cost per treatment analyzes the total cost needed in providing a single treatment or procedure for a patient, and helps to gauge how much investments are needed and in which direction, or whether tweaks are needed in current strategies.
- Why it Matters: It helps providers and payers to identify cost-saving opportunities and helps identify inefficiencies in operations.
- How to Calculate: The total treatment-related costs needed for a single patient for treatment are divided by the number of treatments needed.
- Impact on Healthcare Outcomes: Healthcare organizations can use this data and insight to gain perspective on the ways to make treatments cost-effective while maintaining or improving overall care.
- Best Practices: The insights on costs per treatment help in evaluating the treatment protocols and smoothen operations.
5. Claim Denial Percentage
McKinsey partner Samantha Prymaka highlights that insurers recognize claims as the single most important area through which healthcare payers can gain a sustainable competitive advantage. According to another report by McKinsey, by the end of 2023, 15 % of initial claims were denied for payment. In such a scenario, “digital first” approaches which include dashboards displaying claim denial percentages can prove to be beneficial for speeding up claims processing, tracking fraudulent claims, and understanding claim denials and reasons for the same.
- What it Measures: A healthcare executive dashboard custom-made for measuring claim denials shows the percentage of claims that insurance companies deny.
- Why it Matters: One of the often overlooked aspects of claim management, i.e., denied claims, can delay revenue flow and indicate issues with billing practices.
- How to Calculate: Payers can find the percentage of claims denied by dividing the number of denied claims by the total number of claims made.
- Impact on Healthcare Outcomes: Claim denial can have multiple reasons and both payers and customers might be accountable for the denial or acceptance. However, claim denial can affect cash flow and the overall efficiency of operations.
- Best Practices: To make it easy for the customers and themselves, Payers must improve claim submission accuracy by collaborating with the customer and ensuring proper documentation is submitted and accepted from both ends. This makes the data robust and the claims processing swift.

6. Reimbursement Rate
Gartner highlights the need for CIOs to procure claims-pricing software to simplify reimbursements. Healthcare organizations face the challenge of reimbursements based on care delivered, requiring them to optimize patient outcomes and ensure compliance with value-based care models to maximize reimbursements while maintaining financial stability. Power BI Healthcare dashboards, healthcare financial dashboards, and healthcare compliance dashboards, with reimbursement rate indicators, are one of the important components of such software.
- What it Measures: Claim reimbursement percentage signifies the percentage of healthcare costs reimbursed by the Payer or insurance company.
- Why it Matters: It is critical as it evaluates the financial relationship between the healthcare provider and insurers.
- How to Calculate: It is calculated based on the total reimbursements divided by the total treatment costs.
- Impact on Healthcare Outcomes: A higher claim reimbursement rate is a direct indication of the insurer’s financial performance, viability, and service quality. It helps Payers track which areas need better strategies, which need tweaks, and what’s working for them in general.
- Best Practices: The best way to handle claims reimbursement is by negotiating better contracts and ensuring compliance with billing guidelines.
7. Operating Profit Margin
Healthcare organizations have to look into various costs like operational, clinical, technology, regulatory compliance, reimbursement management, and patient engagement costs. Managing costs and getting ROI is a complex process and requires the assistance of technology and dashboards, which provide real-time analytics, and cost tracking.
- What it Measures: Operating profit margin is a KPI that shows the profitability of a healthcare organization after covering operating costs, taxes, and interest.
- Why it Matters: Operating costs can help an organization determine the efficiency of its operations and processes and manage costs, thus helping pivot strategies or make amends to existing investments.
- How to Calculate: Operating costs are calculated by dividing the profit earned by the total revenue.
- Impact on Healthcare Outcomes: A healthcare KPI dashboard that displays the operating costs ensures the organization has the funds to improve care and expand services.
- Best Practices: Patient care quality is a primary concern and the focus should be on cost-cutting measures without compromising patient care quality.
8. Medical Equipment Utilization
Medical devices are a primary part of caregiving and when used efficiently can be used to improve patient outcomes, and enable less invasive treatments. Additionally, proper utilization can also be a way to ensure that the right facilities reach the right patients and the equipment doesn’t lie unused when the patients are in dire need of it.
- What it Measures: Medical equipment utilization is a KPI that shows the efficiency of medical equipment usage in a healthcare facility. It indicates how often and effectively equipment is used for patient care.
- Why it Matters: Medical equipment is investment-heavy and proper utilization of this equipment minimizes idle time, reduces maintenance costs, and boosts patient throughput. This helps ensure that there is a high return on investment for expensive medical devices.
- How to Calculate: The medical equipment utilization is based on the percentage arrived at by dividing the data received about the total usage time of the equipment and the available equipment time
- Impact on Healthcare Outcomes: Healthcare organizations can use this data to reduce patient wait times, prevent equipment shortages, and ensure timely diagnostics and treatments. Patients can benefit from the improved care and hospital efficiency.
- Best Practices: The best way to ensure accuracy is by tracking equipment usage with IoT-enabled monitoring systems and implementing predictive maintenance to prevent downtime.
Break down data silos and elevate your healthcare analytics with custom-made Power BI healthcare dashboards!
9. Average Hospital Stay
Data reveals that the number of days a patient remains in the hospital is not only based on the criticalness of the disease but also is an indicator of the efficiency of the provider. Data from the National Institutes of Health states that a reduced length of stay can directly reduce the risk of infection, and medication side effects, and result in increased hospital profit.
- What it Measures: It measures the average number of days a patient stays in the hospital right from the first day of admission to the time of discharge.
- Why it Matters: It stands as an indicator of the expertise of the healthcare professionals and affects the reputation of the hospital. It also helps assess hospital efficiency and resource utilization, as longer stays indirectly indicate inefficiencies, higher costs, or complications, while a shorter stay can make resources available for new patients in need of care.
- How to Calculate: The average Hospital stay depends on data received from electronic health records (EHRs), admission-discharge-transfer (ADT) systems, bed management systems, and patient billing systems, to the dashboard about the total inpatient days, and the number of discharges. The average hospital stay is calculated based on the total number of discharges and total inpatient days.
- Impact on Healthcare Outcomes: If the organization manages to get an idea about the average stay, it can help allocate resources like beds, and ICUs effectively, and lower average stays can improve bed availability and reduce costs. On the other hand, a longer stay may indicate complications, increasing patient risk and resource strain, which directly impacts patient satisfaction and hospital revenue.
- Best Practices: The best dashboards are driven by implementing predictive analytics to anticipate patient discharge needs, and enhance care coordination to prevent delays.
10. Readmission Rate
Readmissions, though profitable, can turn out to be an out for punitive action for healthcare organizations. A report by Statista reveals that in 2022, from the 3,046 hospitals that Medicare assessed for hospital readmissions, 42% were penalized for readmission rates exceeding 30-day risk-standardized readmission rates. A dashboard indication of the readmission rates can help providers assess the reason for readmission, find if the need is valid, gauge the competency of healthcare professionals, and identify gaps in discharge planning and follow-up care.
- Why it Matters: It is a clear indicator of the level and quality of care and the effort put into the discharge planning. Additionally, high readmission rates may signal poor patient outcomes and ineffective post-discharge follow-up.
- How to Calculate: The calculation of the readmission rate is done on the dashboard by calculating and comparing the number of readmissions within 30 Days with the total number of discharges within these days.
- Impact on Healthcare Outcomes: A lower readmission rate is a positive indicator of the correct diagnosis and treatment by the healthcare professional, better post-discharge care, and patient adherence to treatment. The high rates can increase costs, reduce hospital ratings, and impact reimbursements.
- Best Practices: The best practices include improving the way discharges are planned and how the patients are educated about post-discharge care. Remote monitoring and telehealth follow-ups are also key aspects that ensure that the health systems are not overwhelmed and loaded for cases where online consultation can give the right direction.
Accelerating Healthcare Growth with High-End KPI Dashboards
Healthcare KPI dashboards have moved from a space of basic medical data visualization to advanced, AI-driven analytics and now act as potent tools for reducing readmission rates, optimizing bed occupancy, improving staff productivity, and boosting patient care coordination. The healthcare compliance dashboard with the above KPIs helps healthcare organizations achieve numerous feats ranging from reducing readmission rates, avoiding Medicare penalties, and optimizing ICU and general ward bed occupancy.
However, getting the most out of your investments in a healthcare executive dashboard goes beyond data visualization—it requires the expertise of a competent dashboard development and analytics team like X-Byte Analytics that can smoothen the integration with your systems, using real-time analytics, and AI-driven insights.
At X-Byte, our experts help incorporate healthcare dashboards in Power BI using advanced data integration capabilities, AI-driven analytics proficiency, and a strong understanding of regulatory compliance to ensure that every healthcare organization we work with can make data-driven decisions and set new benchmarks of excellence. Collaborate with X-Byte to smoothen healthcare workflows, and turn industry-specific challenges into opportunities for growth.






